[ad_1]
The choice of whether to use granulocyte colony-stimulating factor (G-CSF) for the prevention of febrile neutropenia for patients undergoing chemotherapy depends on whether it is being used for primary or secondary prophylaxis, indicates a survey of French clinicians.
The results showed that for primary prophylaxis, the number of injections and the cost of each treatment cycle were key factors in the decision.
Although those factors were also important regarding secondary prophylaxis, more important in the secondary setting was the clinical efficacy of G-CSF.
For either primary or secondary prophylaxis, physicians accepted the use of a biosimilar drug, although such use was a significant factor in secondary prophylaxis only for physicians working in public hospitals.
The results were presented at the recent World Conference on Lung Cancer (WCLC) 2020 by Christos Chouaïd, MD, from the Department of Pneumology, Intercommunal Hospital Center of Créteil, Créteil, France.
His team surveyed 205 oncologists, pulmonologists, and gastroenterologists regarding the factors that influence their decision to use G-CSF.
Chouaïd told Medscape Medical News that he believes that in primary prophylaxis, the choice as to whether to use G-CSF is determined by factors other than clinical efficacy, because in primary prophylaxis, a clinical problem that might be addressed by using G-CSF has not yet arisen.
However, “secondary prophylaxis is, by definition, after febrile neutropenia [occurs],” and so efficacy “becomes important.”
These results are “practice reinforcing, in the sense that most prophylaxis, including G-CSF, is driven by preferences that depend on underlying clinical context,” commented Sandip P. Patel, MD, medical oncologist and associate professor of medicine, UC San Diego Health, San Diego, California, who was not involved in the survey.
The results show that secondary prophylaxis “is driven by efficacy,” whereas primary prophylaxis is driven by safety and/or cost “to prevent a theoretical negative outcome,” which are “reasonable preferences to have,” Patel told Medscape Medical News.
Patel continued: “For many patients, G-CSF is harder on their quality of life than the chemotherapy itself.
“While febrile neutropenia is a major health hazard, it is relatively rare in many populations that receive all the side effects of G-CSF, with less of the benefit,” he said.
He therefore believes that “giving G-CSF to patients who had complications of neutropenia is less controversial, in the sense that we are selecting for a population that will benefit, despite the side effects.”
Table of Contents
Substantial Costs
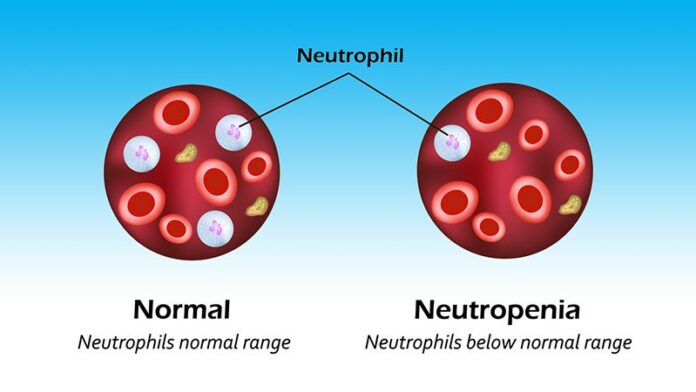
In his presentation, Chouaïd noted that febrile neutropenia is common among cancer patients who undergo treatment with myelosuppressive chemotherapy and is potentially life threatening. Up to 30% of patients experience serious complications; the mortality rate is 11%.
Febrile neutropenia can also have a “substantial” economic impact. In the inpatient setting, it can lead to delays in patient management that cost approximately $16,400 (€13,500) per hospitalization.
Although G-CSF is recommended for the prevention of febrile neutropenia in patients receiving chemotherapy who have a >20% risk for the complication, patients whose risk is 10% to 20% should undergo assessment of patient and disease characteristics, he suggested.
Chouaïd said that a number of studies have indicated that G-CSF is “misused” in clinical practice. It is overused for patients at low or intermediate risk for febrile neutropenia, and it is underused for those at high risk.
The survey that he presented at the meeting was conducted between September 2018 and July 2019.
A discrete-choices-experiment methodology was used in the survey. In such surveys, pairwise comparisons of treatment choices combine various attributes to force respondents to make trade-offs.
In the study, the attributes relating to G-CSF choice were the risk for febrile neutropenia, the use of biosimilars, the cost per treatment cycle, the number of injections per cycle, the degree of injection site pain, bone pain, and influenzalike illness.
The respondents were presented with eight scenarios in which to choose between competing treatments for both primary and secondary prophylaxis.
There were 205 respondents to the survey; 61% were men, and the majority (73.2%) were working in public hospitals. The level of experience was 10 years or less for 40.5% of respondents; 36.1% had 11 to 20 years of experience; and 23.4% had at least 21 years of experience.
For primary prophylaxis, the factors most significantly associated with physician choice were the number of injections per cycle (coefficient, 0.21; P < 10-4) and the cost per treatment cycle (coefficient, 0.11; P < 10-4).
Injection site pain was a lesser consideration (coefficient, 0.08; P < 10-4), as was the efficacy of the treatment, expressed as the risk of developing febrile neutropenia (coefficient, 0.04; P = .015).
Interestingly, the use of a biosimilar was well regarded for primary prophylaxis (coefficient, 0.014; P < 10-4).
Further analysis suggested that, although the criteria for choosing a G-CSF for primary prophylaxis were broadly similar between physicians in public hospitals and those in private hospitals, the risk for febrile neutropenia was a consideration only for those working in public hospitals
For secondary prophylaxis, the number of injections per cycle remained important (coefficient, 0.14; P < 10-4), as did the cost per cycle (coefficient, 0.11; P < 10-4). The risk for febrile neutropenia was a far greater consideration in secondary prophylaxis than in primary prophylaxis (coefficient, 0.09; P < 10-4).
The risk for injection site pain was less relevant to physicians with regard to secondary prophylaxis (coefficient, 0.05; P = .005), but the use of biosimilars remained a welcome option (coefficient, 0.11; P < 10-4).
The importance of the various criteria for choosing a G-CSF for secondary prophylaxis of febrile neutropenia were again similar between physicians who worked in public hospitals and those who worked in private hospitals, although the use of biosimilars appeared to be more relevant for those in public hospitals.
Impact on Mortality?
Chouaïd noted that it would be “interesting” to determine whether the convergence of physician preferences seen over the choice of G-CSF in the primary and secondary settings “has an impact on the mortality rate linked to the occurrence of febrile neutropenia during a cycle of chemotherapy.”
Patel agreed, saying that a study of the factors that lead to G-CSF being withheld in high-risk individuals, in association with mortality rates, “could be important, as these patients should be receiving G-CSF primary prophylaxis.”
No funding for the study has been reported. Chouaid has relationships with Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, GSK, Janssen, Lilly, MSD, Mundipharma, Novartis, Sanofi Aventis, and Roche.
World Conference on Lung Cancer (WCLC) 2020: Abstract FP06.01. Presented January 28, 2021.
For more from Medscape Oncology, join us on Twitter and Facebook.
[ad_2]
Source link