[ad_1]
Combining standard neoadjuvant chemotherapy for locally advanced esophageal cancer with either radiation or docetaxel did not increase the risk of surgical complications, investigators in the JCOG1109 trial reported.
The trial included patients with clinical stage IB, II, or III (non-T4) thoracic esophageal cancer randomly assigned to cisplatin plus 5-fluorouracil (CF), CF plus radiotherapy (CF-RT), or docetaxel plus CF (DCF) prior to surgery.
Results showed the type of therapy did not significantly affect risk for either perioperative complications or deaths. There was also evidence to suggest that a lower risk of postoperative complications with DCF compared with CF might translate into improved prognosis with the addition of docetaxel, said Kazuo Koyanagi, MD, PhD, of National Cancer Center Hospital in Tokyo.
Koyanagi presented these results at the 2021 Gastrointestinal Cancers Symposium.
“Based on these results, we could say that preoperative chemotherapy with DCF and CF-RT didn’t increase the risk of postoperative complications when compared with standard CF, and whether the decrease in the risk in the DCF would be reflected in the improvement of prognosis should be examined in the future,” Koyanagi said.
Table of Contents
Trial Details
The JCOG1109 trial is a three-arm, phase 3 trial designed to see whether adding docetaxel or radiation to CF could improve outcomes. In the analysis presented here, the investigators examined whether the choice of regimen could affect the safety of esophagectomy, and they looked for risk factors for postoperative complications.
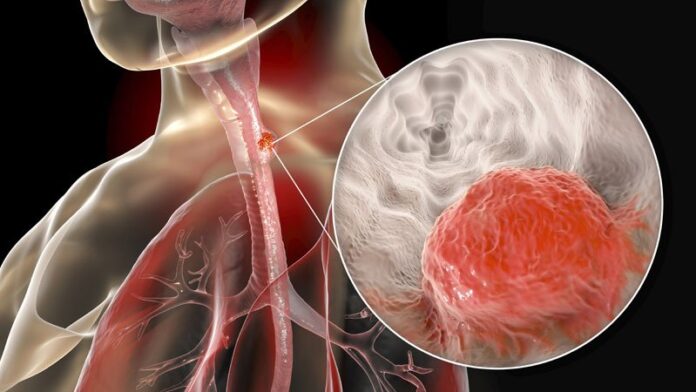
Patients with histologically proven squamous cell, adenosquamous, or basaloid carcinoma with locally advanced lesions in the thoracic esophagus were eligible.
The patients had to have good performance status (Eastern Cooperative Oncology Group 0 or 1) and could not have had chemotherapy, radiotherapy, or hormonal therapy for any cancer, or prior therapy for esophageal cancer except for complete endoscopic mucosal or submucosal dissection.
A total of 601 patients were enrolled and randomized to receive one of the following treatments:
-
CF, with cisplatin at a dose of 80 mg/m2 on day 1 and 5-fluorouracil at 800 mg/m2 on days 1-5 every 3 weeks for two cycles (199 assigned; 185 had surgery)
-
DCF, with cisplatin at 70 mg/m2 on day 1, 5-fluorouracil at 750 mg/m2 on days 1-5, and docetaxel at 70 mg/m2 on day 1 every 3 weeks for three cycles (202 assigned; 183 had surgery)
-
CF-RT, with cisplatin at 75 mg/m2 on day 1, 5-fluorouracil at 1,000 mg/m2 on days 1-4 every 4 weeks for two cycles, plus 1.8 Gy radiation divided into 23 fractions for a total of 41.4 Gy (200 assigned; 178 had surgery).
Patient age, body mass index, tumor location, clinical stage and node status were comparable among the treatment groups.
Operative characteristics (duration, blood loss, approach, extent of lymph node dissection) were generally similar between the arms as well, except that significantly fewer lymph nodes were harvested with CF-RT compared with either CF or DCF (median of 49, 58, and 59, respectively).
Results
Incidence rates of major postoperative complications – pneumonia, leakage, and recurrent laryngeal nerve paralysis – were generally similar among the groups.
The cumulative rate of grade 2 or greater postoperative complications was significantly lower for DCF than for CF (P = .02), but not for DCF compared with CF-RT (P = .11). The rates were 43.7% with DCF, 47.8% with CF-RT, and 56.2% with CF.
The rate of grade 2 or greater chylothorax (leakage of lymphatics into the pleural space) was significantly higher with CF-RT than CF (5.1% vs. 1.1%, P = .03) but not with DCF vs. CF (3.8% vs. 1.1%, P = .10)
In multivariable analysis controlling for demographic, clinical, and operative characteristics, factors associated with lower risk for complications included:
-
Middle esophageal tumor location vs. upper esophageal tumors (relative risk [RR], 0.79; P = .03)
-
DCF (RR, 0.79; P = .02)
-
A thoracoscopic vs. open approach (RR, 0.77; P = .002).
The only factor associated with higher risk was operative time longer than 492 minutes (RR, 1.26; P = .008).
Koyanagi said the reasons for the lower lymph node yield and more frequent chylothorax with CF-RT are unclear but may be related to tissue fibrosis from radiation exposure.
CROSS Talk
“As a North American surgeon, I generally look to CROSS induction chemotherapy for the majority of my patients for both adenocarcinoma and squamous cell carcinoma of the esophagus,” said invited discussant Jonathan Yeung, MD, PhD, of the Princess Margaret Cancer Centre in Toronto.
The CROSS regimen consists of carboplatin titrated to an area under the curve of 2 mg/mL per minute and paclitaxel at 50 mg/m2 for 5 weeks with concurrent radiotherapy to a total dose of 41.4 Gy delivered in 23 fractions, 5 days per week.
Yeung noted that, of the eligible patients in JCOG1109, 92% of those assigned to DCF actually underwent surgery, and 90% of those assigned to CF-RT went on to surgery, compared with 98% of patients who had surgery in the CROSS trial, suggesting that the DCF and CF-RT regimens may be more toxic.
He also noted that the lower lymph node harvest seen with CF-RT was seen in other studies.
“I must say I’m always impressed by the lymph node yields that our Japanese colleagues can obtain at surgery, but this lower lymph node yield is also borne out in the CROSS data, where there are less lymph nodes harvested following chemoradiotherapy,” he said.
A higher rate of chylothorax with CF-RT was also seen in patients in the CROSS trial who were randomized to receive radiation compared with those who received chemotherapy alone.
“I await the final results to see if there is ultimately better survival,” Yeung said.
JCOG1109 was supported by grants from the National Cancer Center Research and Development Funds and Agency for Medical Research and Development of Japan. Koyanagi and Yeung reported no conflicts of interest.
The Gastrointestinal Cancers Symposium is sponsored by the American Gastroenterological Association, the American Society for Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
This article originally appeared on MDedge.com, part of the Medscape Professional Network.
[ad_2]
Source link