[ad_1]
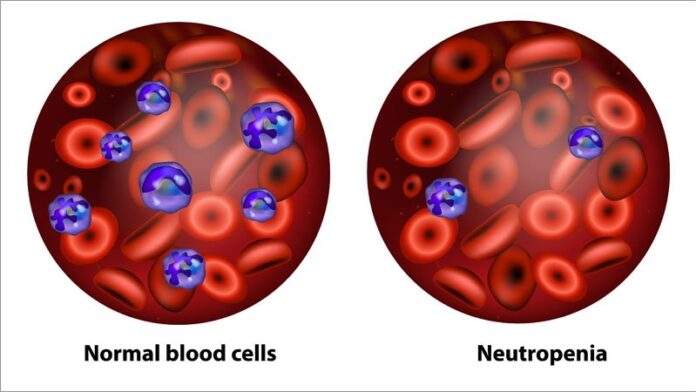
In the United States, for the past two decades, pegfilgrastim (Neulasta) and its biosimilars have been the widely used standard of care for the prevention of chemotherapy-induced neutropenia (CIN).
Now, the champions of a new agent, plinabulin (BeyondSpring), say that adding it to pegfilgrastim represents a “major advancement” and a “new paradigm” in preventing such neutropenia.
But experts contacted by Medscape Medical News have doubts.
The enthusiastic comments about plinabulin appear in a company press release, issued to highlight topline results from a phase 3 trial in breast cancer. Data from this trial were presented in a poster at the recent San Antonio Breast Cancer Symposium (SABCS) 2020.
Some of the comments come from the trial’s principal investigator, Douglas Blayney, MD, of Stanford University, Palo Alto, California, a former president of the American Society of Clinical Oncology.
In an interview, Blayney said there is room for improvement in the prevention of neutropenia.
Currently, the main treatment is with growth colony-stimulating factors (GCSFs). The first of these, filgrastim, “was a great advance in the 1990s when it decreased incidence of neutropenia ― but it didn’t make it go away,” he said.
Since then, filgrastim has largely been superseded by pegfilgastim, which needs to be given only once in a cycle of chemotherapy, rather than every day.
But a GCSF “does not eliminate neutropenia, it only reduces the depth of the neutropenia,” Blayney explained.
Plinabulin is not a GCSF ― it’s an experimental small molecule that was first tested more than 10 years ago as an anticancer therapy and was observed in clinical trials to maintain white blood cell counts after chemotherapy, Blayney said last year in an interview.
Plinabulin has subsequently been investigated for use in the prevention of CIN, including in a registration trial for a specific breast cancer regimen.
That phase 3 trial, known as PROTECTIVE-2, was conducted among 221 breast cancer patients being treated with docetaxel, doxorubicin, and cyclophosphamide. All study patients received pegfilgrastim, the standard of care for the prevention of neutropenia. They were also randomly assigned to receive either plinabulin (n = 111) or placebo (n = 110) on day 2 of the first treatment cycle.
The primary endpoint of the trial was the rate of prevention of grade 4 neutropenia, which was reported as occurring in 31.5% of patients who received the combination of plinabulin plus pegfilgrastim, vs 13.6% of those who received pegfilgrastim monotherapy (P = .0015).
In their poster at SABCS, the authors report that the plinabulin arm “was associated with a >40% reduced febrile neutropenia risk” compared to the placebo arm (19.7% vs 40.9%; odds ratio, 0.592).
In the company press release issued in November, Blayney said, “The combination of plinabulin with pegfilgrastim represents a major advancement in offering protection against CIN…..” The company chief medical officer, Ramon Mohanlal, MD, PhD, declared that “plinabulin represents a new treatment paradigm for CIN prevention….”
However, that would-be advance may or may not include a documented significant reduction in the rate of febrile neutropenia, because in the poster presentation, the actual number of patients with fever was not given.
Blayney said the full tally of the number of patients with febrile neutropenia in the breast cancer trial was not complete and that the final data were not available because the trial had only been completed a month earlier.
“Preliminary results of a randomized phase 3 trial show that we are on the right track [with regard to CIN],” he told Medscape Medical News.
Table of Contents
How Important Is Febrile Neutropenia?
An expert who was approached for comment, Terry Ng, MD, medical oncologist, University of Ottawa, Ontario, Canada, said the results of the breast cancer study are not entirely clear, inasmuch as the endpoint ― the rate of prevention of grade 4 neutropenia ― is not easily understood and does not represent what is most clinically significant.
“It’s somewhat confusing the way that they worded it,” Ng told Medscape Medical News. “I don’t understand how you would calculate the rate of prevention of grade 4 neutropenia.”
Blayney did not respond to a subsequent Medscape Medical News request to explain the endpoint.
Ng said that grade 4 neutropenia is a not an optimal primary outcome because not all such cases result in fevers and infection. The most clinically important measures, he said, are the rates of febrile neutropenia, hospitalization, and sepsis.
Agreed, said Charles Shapiro, MD, medical oncologist, Icahn School of Medicine at Mount Sinai, New York City, who was also asked for comment.
“What counts most is neutrophils <500/uL and fever, or febrile neutropenia,” Shapiro told Medscape Medical News.
Shapiro believes any would-be addition to pegfilgrastim should require strong supporting evidence, because alone, it is “already good at reducing the incidence and duration of febrile neutropenia and severe neutropenia.”
National Comprehensive Cancer Network (NCCN) guidance supports Ng’s and Shapiro’s points of view on the importance of febrile neutropenia.
GCSFs “are primarily used to reduce the incidence of febrile neutropenia,” reads the NCCN’s guidelines for myeloid growth factors. Prophylactic usage is “based on risk assessment for febrile neutropenia” among patients with solid tumor receiving myelosuppressive chemotherapy, it also states.
In addition, the NCCN further explains the significance of fevers associated with the depletion of neutrophils: “Febrile neutropenia [FN] is a major dose limiting toxicity of many chemotherapy regimens. Patients who develop FN often require prolonged hospitalizations and treatment with broad-spectrum antibiotics. Development of FN increases treatment costs and can prompt dose reductions or treatment delays, which may compromise clinical outcome.”
However, in the PROTECTIVE-2 trial of plinabulin, febrile neutropenia is not listed as a secondary outcome, suggesting that that endpoint is not deemed necessary for approval of the drug by the US Food and Drug Administration (FDA).
The omission of febrile neutropenia as an endpoint in plinabulin’s phase 3 breast cancer trial is an approach supported by the approval of pegfilgrastim (Neulasta) in 2002. The primary endpoint for its two pivotal studies was the duration of severe neutropenia. According to the FDA prescribing information, the use of that outcome is based on the “correlation between severe neutropenia and the incidence of febrile neutropenia” found in earlier studies of filgrastim, the predecessor of pegfilgrastim.
“Interesting Drug…. Might Have a Role”
“I am very nonplussed about the agent,” said Shapiro, who is director of translational breast cancer research for the Mount Sinai Health System, when asked for an opinion about plinabulin data presented in the SABCS poster.
Ottawa’s Ng does not dismiss plinabulin as a treatment for the prevention of CIN, including in breast cancer and possibly other cancers.
Plinabulin is an “interesting drug,” Ng said in an interview. He cited a phase 2 study published last year in JAMA Oncology. That study was a head-to-head comparison of plinabulin vs pegfilgrastim for protection against CIN among lung cancer patients receiving platinum-based chemotherapy. Plinabulin was found to be noninferior to pegfilgrastim.
What most caught Ng’s eye were findings other than those related to efficacy.
The rate of bone pain, a “major” side effect of pegfilgrastim, was significantly less, and quality of life was improved with the experimental agent, he said. “That’s really important because there are still high-risk patients that need chemotherapy ― many of them will receive the chemotherapy…and experience significant bone pain [with GCSF],” Ng commented.
Plinabulin might have a role in chemotherapy-induced neutropenia.
“So I do think plinabulin might have a role in chemotherapy-induced neutropenia,” he summarized.
However, Ng said that in general, it was “not clear” whether plinabulin should be administered as a single agent in place of pegfilgrastim or whether it should be combined with the GCSF.
There are also financial considerations. On its own, pegfilgrastim is already costly, he said, echoing comments from Shapiro, who called for an eventual cost-effectiveness study of plinabulin.
Whether or not an agent “like plinabulin should become standard of care for prophylaxis” will necessitate “longer-term results and, most importantly, cost-effective analyses that will need to be done by experts,” said Ng.
The breast cancer study was funded by BeyondSpring, which owns plinabulin. Blayney has received financial support for travel and lodging from the company. Ng and Shapiro have disclosed no relevant financial relationships.
San Antonio Breast Cancer Symposium (SABCS) 2020: Abstract PS11-15. Presented December 9, 2020.
Nick Mulcahy is an award-winning senior journalist for Medscape. He previously freelanced for HealthDay and MedPageToday and had bylines in WashingtonPost.com, MSNBC, and Yahoo. Email: [email protected] and on Twitter: @MulcahyNick.
For more from Medscape Oncology, join us on Twitter and Facebook.
[ad_2]
Source link