[ad_1]
Editor’s note: Find the latest COVID-19 news and guidance in Medscape’s Coronavirus Resource Center.
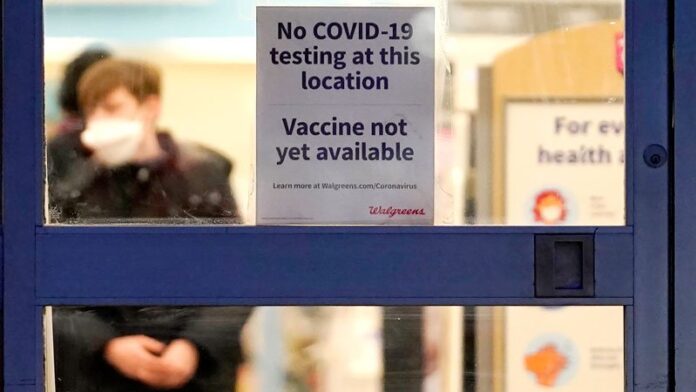
Physician offices, which have been deemphasized in the COVID-19 vaccine rollout, should have a more prominent role in the effort going forward, said the Medical Group Management Association (MGMA) in a letter sent to President Joe Biden on Tuesday.
“Due to our members’ role as community providers, we ask that the Administration include medical group practices in COVID-19 vaccine distribution strategies moving forward,” stated Halee Fischer-Wright, MD, president and CEO of MGMA, in the letter.
“Current vaccine efforts are haphazard at best and appear to rely on a passive first come first served approach with the public rushing to sign up for vaccines when scant supply becomes available,” MGMA noted. “This favors patients who can advocate for themselves or have family members able to do the same. Yet medical group practices already have patient relationships and experience vaccinating patients for influenza and other conditions.”
Moreover, physician practices have data on patient demographics, preexisting conditions, and risk factors. This is valuable information not available to hospitals, pharmacies, and state health departments, MGMA said.
“Furthermore, in a time of uncertainty and misinformation, patients are looking to their own physicians as a trusted source for information on vaccine safety and efficacy,” the letter stated. “Physician group practices can and should play a significant role in vaccine education.”
Despite these advantages of vaccinating patients in doctors’ offices, MGMA pointed out: “states have largely not leveraged physician practices in vaccine rollout efforts.”
In an MGMA survey conducted last week, 85% of independent practices and 45% of hospital- or health system-owned practices that sought COVID-19 vaccine for their patients were unable to obtain any. Of the practices able to get vaccine supplies, the majority said they had received only enough to vaccinate 1% or less of their patients.
Susan R. Bailey, MD, president of the American Medical Association commented in an email to Medscape Medical News: “Once enough supplies are available, we encourage the Administration to ensure physician practices have an adequate supply of COVID-19 vaccines to vaccinate their patients. Physician practices will be an integral part of the vaccine administration process. Physicians are a trusted source of information for patients and their direct conversations and recommendations for patients to get vaccinated will help address hesitancy and result in more people getting vaccinated.”
Many groups, MGMA said, had been approved by their states to distribute the vaccine but received little or no inventory. Practice phone lines have been “flooded” by patients wanting to know why their physicians can’t vaccinate them.
Table of Contents
Programs Vary By State
In an interview with Medscape Medical News, Fischer-Wright said most practices want to vaccinate their patients. But only some states have set up programs that allow them to apply for the COVID-19 vaccines. “Most of our practices that were eligible for vaccination have applied for it,” she said.
The New York State Health Department is taking a different approach, according to Dial Hewlett, Jr, MD, medical director for disease control services with the Westchester County Department of Health in White Plains, New York. The state health department has designated specific sites across New York as vaccination hubs; in Westchester County, the hub is the Westchester Medical Center. When the hospital receives a vaccine shipment, it distributes some of it to smaller sites such as the county health department, which includes a vaccination clinic.
“So far, they haven’t gotten to the point where they’re distributing to pharmacies or doctors’ offices,” Hewlett told Medscape Medical News.
Right now, he said, the chief limiting factor is vaccine supply. When that expands, he said, physician offices will likely get more vaccine doses.
Both Hewlett and Fischer-Wright point out that physician offices are limited because they aren’t able to store the Pfizer vaccine, which requires ultra-cold freezers. “But now that we have the Moderna vaccine, 50% of the 200 million doses that have been promised can be delivered in a physician office,” said Fischer-Wright.
So why haven’t practices received more vaccine? Besides the inadequate supply across the nation, Fischer-Wright said, there have been difficulties in getting the vaccine to physician offices. Some MGMA members, she added, did receive vaccine supplies immediately. “These were independent practices that had over 200 physicians,” she said.
Hewlett noted that some smaller practices have complained to the county department that they couldn’t obtain vaccine because they lacked the clout to compete with larger groups. “They’re not ordering enough product to make it a priority for whoever is involved with the distribution,” he said.
Another problem — evident in the results of MGMA’s recent poll — is that healthcare systems that have vaccine supplies are sharing them with their own practices before they make any available to community practices.
“If you’re working for Northwell Health, you probably won’t have the kinds of challenges that the small mom-and-pop practice would have,” Hewlett said.
Overcoming Vaccine Hesitancy
More than a quarter of the US population has indicated they are hesitant to get the COVID-19 vaccine. This is an area where Fischer-Wright believes physicians can help immensely.
“The benefit of having that type of activity occur in the physician office is that it’s a place where physicians have already established trust with patients,” she said. “And one of the reasons why some people don’t want a shot is that they don’t trust the vaccine. Having a human being that you have a relationship with provide you with the pros and cons is very compelling to get people to make an alternative choice.”
Physicians and their staff will also need to be educated before they administer the vaccine, Hewlett noted. “There will have to be education on the handling of the vaccine, but I think that can easily be done,” he said. “Many practices have physician assistants and nurse practitioners who have been doing a lot of vaccinations in the office setting.”
Complex Logistics
Based on the experience of his department’s vaccination clinic, which has been giving COVID-19 shots since January 5, Hewlett said private practices have a lot to consider before they launch their own vaccination efforts.
To begin with, he said, “it’s a tricky situation with these vaccines that require two doses.” Before his clinic makes an appointment to vaccinate a patient, he noted, the scheduler has to make sure that the patient can return in 21 or 28 days, depending on whether they’re getting the Pfizer or Moderna vaccine.
“It’s difficult if they can’t show up 28 days after that date because we expect the same number of people to show up 28 days later for their second dose,” he said. “This is quite different from a standard medical practice. There aren’t too many situations where a person has to come back to the office after 28 days or 21 days.”
While the Centers for Disease Control and Prevention recently said the immunization schedule can be more flexible, Hewlett added, his clinic prefers to get patients back on the recommended schedule to make sure the vaccine will be maximally effective.
The clinic also has to follow state regulations requiring that all vaccines it receives be administered within a week of receipt. Right now, the clinic is open six days a week, giving about 300-400 shots a day. Each morning, a clerk records how many doses were administered the previous day, along with the lot numbers — and all data must be reported to the state.
The operation is fairly labor intensive. The clinic has a staff of about 30 people, most of whom are now engaged full time in the COVID-19 vaccination effort.
“We have people who check patients in and who screen to make sure no one has COVID symptoms. Other people escort patients to the vaccination stations. We have about 15 nurse practitioners and public health nurses who give the shots, and we have to make sure they’re accounting for every dose that’s given. And we have to make sure everybody getting a dose meets the eligibility criteria for shots,” he said. “We also have an area where patients are watched for 15 minutes after they’re vaccinated. Then there’s a group of five data entry people who locate appointment slots 28 days from today.”
It’s all still “a work in progress,” Hewlett said, but the staff who give COVID-19 shots and the patients who receive them are gratified to be making a difference.
Follow Medscape on Facebook, Twitter, Instagram, and YouTube.
[ad_2]
Source link